Vestibular Rehabilitation (Dizziness & Balance)
One-on-one assessment and targeted exercises to treat vertigo, dizziness, and motion sensitivity—so you can move confidently again.
Book Now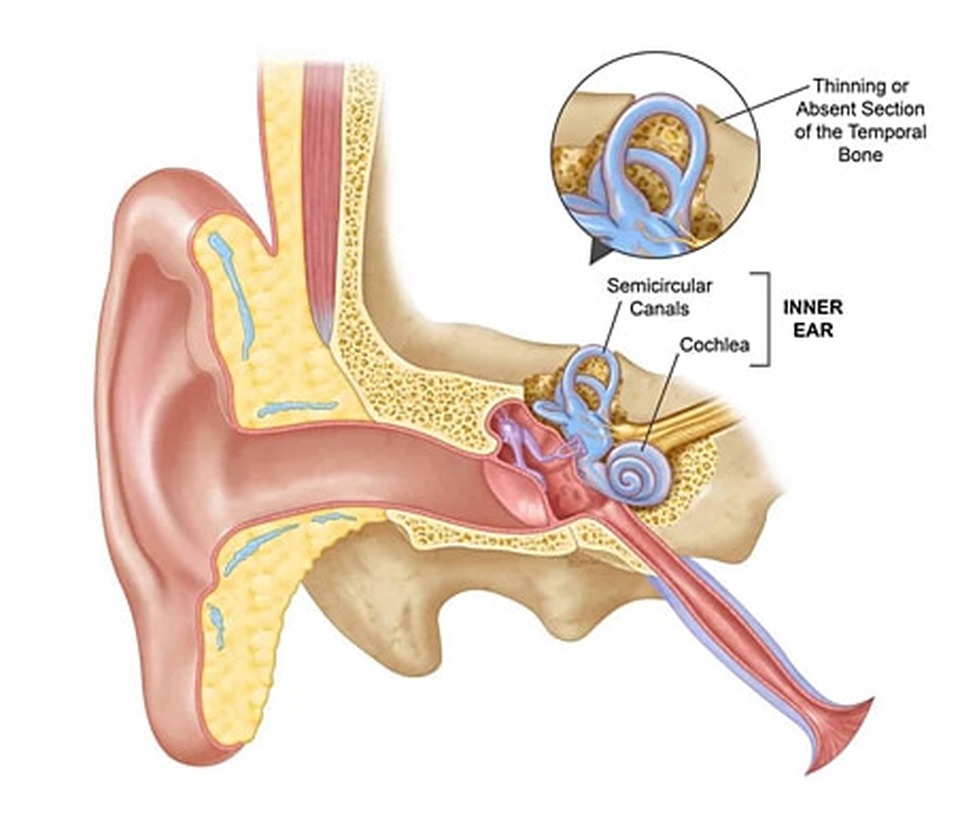
One-on-one assessment and targeted exercises to treat vertigo, dizziness, and motion sensitivity—so you can move confidently again.
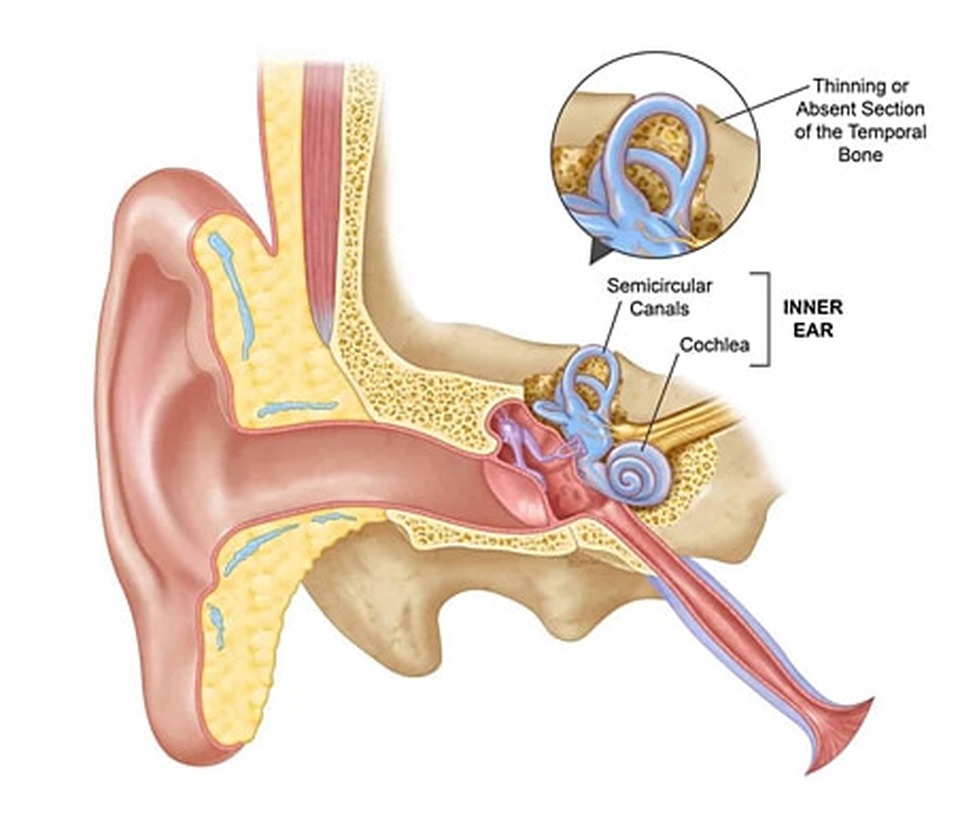
Book NowThe vestibular system (inner ear, eyes, and brain) keeps you steady and oriented. Injury or dysfunction can cause vertigo, dizziness, imbalance, nausea, and “busy background” blur. Vestibular rehabilitation uses specific maneuvers and exercises to retrain this system.
BPPV: many improve in 1–3 sessions; recurrences are common but usually resolve quickly with repeat maneuvers and home strategies.
Unilateral hypofunction / neuritis: often 4–8 visits over 4–8 weeks with daily home exercises.
Complex cases (PPPD, post-concussion, Menière’s): usually 6–12+ visits across 8–12+ weeks with careful progression and medical coordination.
Vestibular rehab is safe and effective when tailored to you. Mild temporary dizziness during exercises is expected and part of retraining.
Vestibular therapy provided by licensed physiotherapists is billed as physiotherapy. In NL you can book directly; some plans may require a physician’s referral for reimbursement. We offer Direct Billing to many insurers.
They can briefly provoke vertigo, which is expected, but episodes are short. We guide breathing and pacing to keep you safe.
BPPV often improves immediately or within a few days. Hypofunction and post-concussion dizziness improve steadily over weeks with consistent home practice.
BPPV can recur; we’ll teach recognition and self-care. For other conditions, staying active and continuing a few maintenance drills helps durability.
No imaging is typically required, and you can book directly. If we suspect a medical issue, we’ll liaise with your physician or ENT.
Book your one-on-one vestibular assessment. We’ll confirm the cause and build a plan to help you move with confidence.
Book Now